Hello!
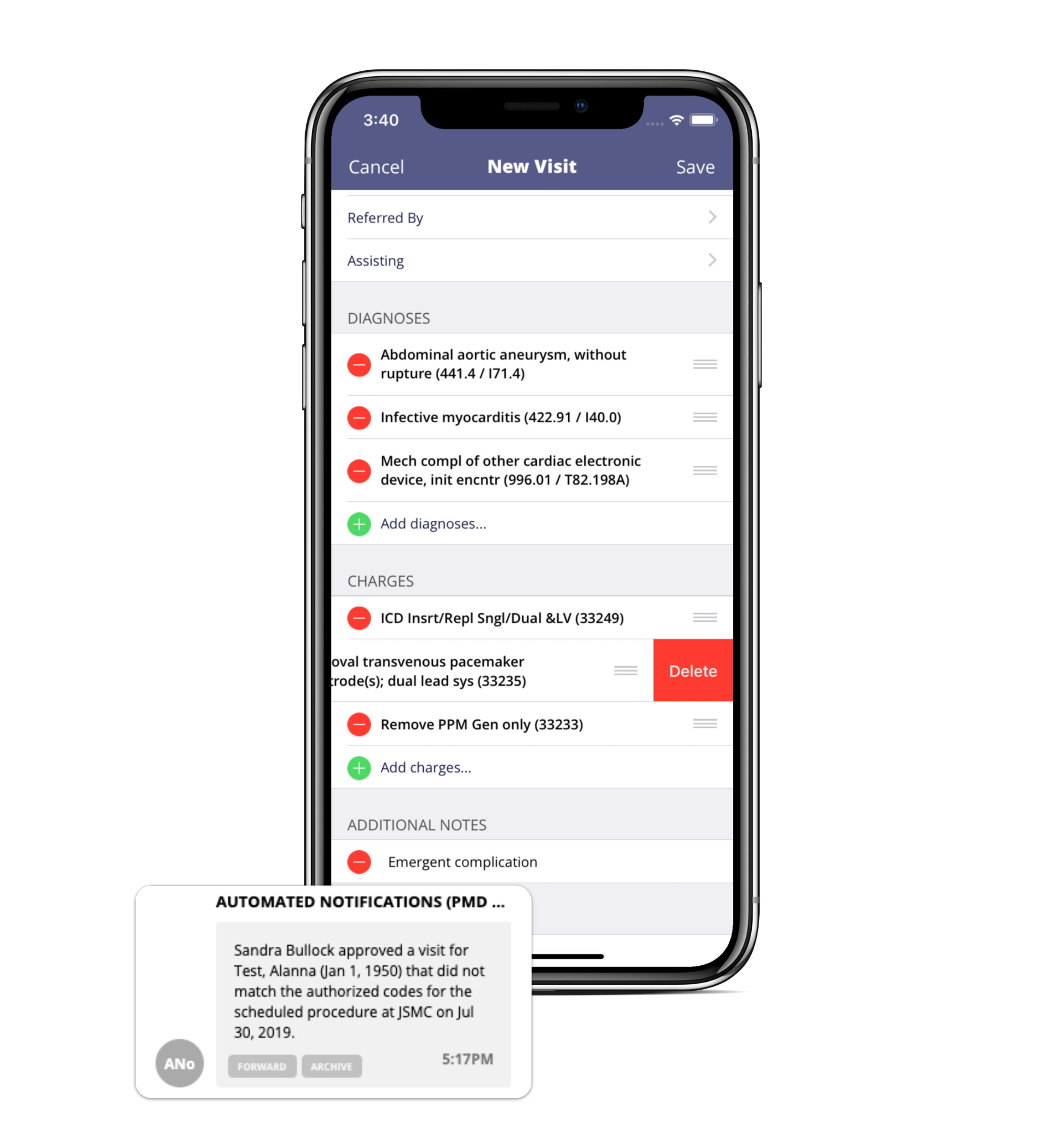
pMD has released a new feature to help notify surgical billing teams when changes to pre-certified surgeries occur. If a complication or last-minute change causes the procedure performed to differ from the pre-certified diagnosis or charge codes, designated staff members can be automatically alerted via pMD secure message.
Some insurance companies allow as little as 24-hour notice to approve changes to an authorization. If a procedure changes or becomes more complex on short notice, these alerts can help practices contact the insurance company as soon as possible to reduce denials and receive reimbursement in a timely manner.
These are currently available for all interested groups. To get started today or to learn more, contact us!
Thank you for using pMD!
Cheers,
The pMD Team
